Invisible Disabilities: Providing First Aid Support


Invisible disabilities are medical conditions that are not immediately apparent to others.
While they may not be visible on the surface, they can significantly affect a person's well-being and functioning.
These disabilities encompass a wide range of conditions, some of which hold great social stigmas or are difficult to diagnose.
As a responsible first aid provider, it is crucial to understand and address the unique needs of individuals with invisible disabilities.
Invisible disabilities come in various forms, and they affect millions of people worldwide. Some common examples include:
You can learn more about invisible or hidden disabilities in our article here: Understanding Invisible Disabilities: A Comprehensive Guide
When it comes to providing first aid for individuals with invisible disabilities, it's essential to adopt a compassionate and inclusive approach.
Many incidences that require first aid are already stressful, so adding an invisible disability to the mix can increase complexity significantly.
After gaining consent to assist, ask the casualty if there are any conditions that you should be aware of. If they do inform you of an invisible disability, ask how best you can help with that in mind. They may prefer a quieter space, or to have you touch them as little as possible.
First and foremost, it's crucial for first responders and medical personnel to educate themselves about various invisible disabilities.
Understanding the symptoms, triggers, and possible complications is vital for effective assistance.
Simple adaptations can be beneficial for many different conditions and can even be beneficial for those with no underlying conditions. E.g. moving to a quieter and more private space is generally preferred by all.
When interacting with someone who has an invisible disability, approach them with respect and empathy.
Ask if they require assistance and listen to their needs without judgment.
Be aware of your voice volume and tone, and move in a gentle way. Be very clear and concise with your explanations.
If their disability impacts communication, adapt your approach to suit. This could include showing items you will be using, rather than speaking about them.
Certain conditions, like sensory processing disorders, can have specific triggers that may exacerbate symptoms.
Be aware of these triggers and try to minimize them whenever possible.
If the casualty is becoming extremely distressed, you could try to offer a distraction. For example if loud noise is a trigger, offer headphones with soothing music, or white noise.
Medical equipment can be a trigger, so you may ask the casualty to look away from what you are doing. Ask if they’d like you to tell them about the items, or if they’d rather not know.
In cases where sensory overload or mental health issues are involved, offering a quiet and calm environment can be immensely helpful.
When safe to do so, find a quite space, preferably inside, and move there.
Ask non-useful bystanders to please move away from the scene, as the casualty is overwhelmed and it is difficult to treat them this way.
If you have any available, you could offer noise cancelling headphones.
For individuals with mobility issues or chronic pain, be prepared to offer physical support when needed, such as helping them sit or lie down comfortably.
Ask what the best way to support them is and be very gentle with your touch.
When dealing with individuals facing mental health challenges, be patient and non-judgmental.
Encourage them to seek professional help if necessary and offer support in finding resources.
Keep a well-stocked first aid kit that includes items like pain relief medications, stress-relief tools (e.g., stress balls), and sensory-friendly items like noise-cancelling headphones or sunglasses.
As someone who may need to provide first aid, recognizing and accommodating individuals with invisible disabilities is a crucial aspect of providing effective care.
By educating yourself and your team, adopting a compassionate approach, and having the right resources on hand, you can make a significant difference in the lives of those with invisible disabilities.
Remember that empathy, patience, and understanding are key when providing first aid support to these individuals, allowing them to receive the care and assistance they need to thrive.

March 25, 2025
Explore non-traditional paths to sobriety, including mindfulness, yoga, nutritional therapy, and community-based support, for a personalized approach to recovery.
September 7, 2022
Menopause is the final period, when a woman, trans man, or non-binary person assigned female at birth's ovaries run out of eggs and the body can no longer ovulate. Menopause comes with several symptoms, complications, and treatment options.
July 26, 2024
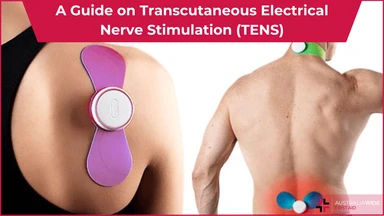
Transcutaneous Electrical Nerve Stimulation (TENS) is a therapeutic method of pain relief. It utilises an electrical device that emits electrical currents and streams the impulses via electrode patches attached to the skin.